Herniated Discs | What Are Your Treatment Options?
What Is A Herniated Disc?
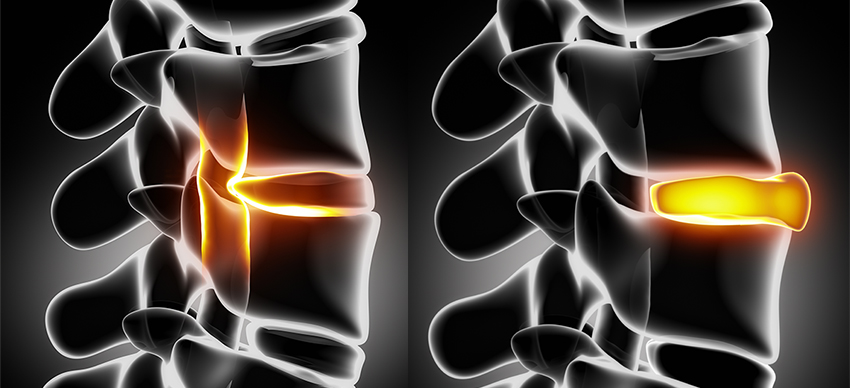
Intervertebral discs are located between each vertebra in the spine and serve as built-in shock absorbers. Each disc is composed of a hard outer shell called the annulus, and a gel-filled interior called the nucleus.
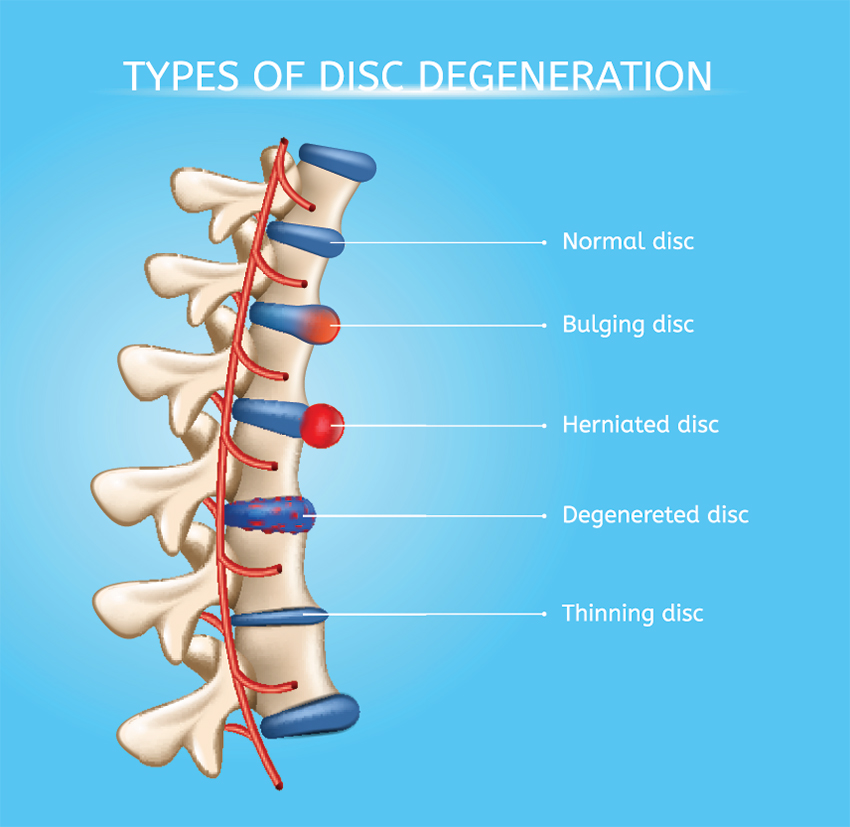
The discs cushion impacts on the spine as the body moves and flexes.
Repeated stresses and gradual wear and tear on the spine, poor posture and degenerative conditions like arthritis can all cause disc degeneration, leading to a bulge or herniation over time. This condition is sometimes referred to as a slipped disc, but discs don’t really slip out of place. Herniate is a more accurate term because stress can cause a crack in the hard outer shell and the inner gel can bulge out through that crack. The gel then presses against nerves, particularly the sciatic nerve, creating pain (known as sciatica) that radiates into the legs.
Typical Symptoms & Diagnosis
Many patients have herniated discs without even knowing it. They experience no pain, but the disc does show up on diagnostic imaging. If you do have pain caused by herniated discs, the pain has a definite pattern–it usually starts near the spine as a dull lower back pain, and then becomes a shooting pain (sciatica) as it travels down into the hips and legs. Muscle spasms and general numbness or weakness often accompanies the pain.
A herniated disc will most often occur in the lower back or neck (cervical spine). The most common symptoms are:
- General weakness. Because the disc is pressing on a nerve, the muscles are not getting a proper nerve signal and tend to weaken over time.
- Pain in the extremities: Lower back herniated discs cause lower back pain, while neck discs cause arm pain. Leg pain can be felt in the thighs, calf and buttocks, or even in the foot. Arm pain is usually most intense in the shoulders.
- Tingling or numbness: The affected nerves cause numbness and tingling in the arms and legs. When you change position or sneeze or cough, you may experience shooting pain caused by nerve irritation.
Diagnosis is usually done by a form of imaging like X-ray, CT scan or MRI.
Treatment
In some cases, a herniated disc will heal on its own. Half of the cases heal within the first month, as inflammation decreases. The doctor will limit your activity or even order bed rest, and may require you to do physical therapy to strengthen your lower back muscles. Core strengthening and activity that doesn’t aggravate pain is extremely helpful. Pain medication may be prescribed, but usually only provides temporary relief and comes with certain side effects. Some patients find relief with corticosteroid injections when the pain is debilitating. Finding ways to manage pain and continue functioning without drugs is ideal. Home electronic stimulation like H-Wave has shown to be particularly useful to reduce pain and swelling. H-Wave’s unique and scientifically proven method of electrical stimulation keeps blood and circulation moving in the area while also producing lasting drug-free pain relief.
Care from a chiropractor can also be helpful, and will likely include a chiropractic adjustment called a spinal manipulation to ease the disc back into its normal position.
When Surgery Is Necessary
Nearly 90 percent of discs heal on their own within six months, but if your disc herniation is more severe, surgical repair might be required. Surgery is usually the best option for people who have suffered a traumatic injury, for cases where nerve damage has occurred, and in cases that haven’t healed in six months with the patient still experiencing significant pain.
There are a variety of surgical options, ranging from minimally invasive to full surgeries. Endoscopic microdiscectomy is a minimally invasive procedure done on an outpatient basis. The procedure is done with a local anesthetic and a sedative; a one-inch incision is made and the disc is repaired; the surgeon will remove the material that has leaked from the inner core of the disc or will push the bulging material back into the disc. The procedure takes about an hour, and patients can begin walking right after surgery with restricted activities for a couple of days.
 A more involved surgery involves complete removal of the damaged disc and replacement with an artificial disc. Artificial discs function just like a natural disc because they are made of cartilage-like tissues. The artificial disc is flexible enough to allow normal range of motion in your spine and neck, and is typically used in cervical and lumbar cases. An abdominal incision is done in the lumbar case and an incision on the front of the neck is done in the cervical case. The surgery is done under general anesthesia and can last three hours. A post-surgery hospital stay is required, and it generally takes several weeks to resume normal activities.
A more involved surgery involves complete removal of the damaged disc and replacement with an artificial disc. Artificial discs function just like a natural disc because they are made of cartilage-like tissues. The artificial disc is flexible enough to allow normal range of motion in your spine and neck, and is typically used in cervical and lumbar cases. An abdominal incision is done in the lumbar case and an incision on the front of the neck is done in the cervical case. The surgery is done under general anesthesia and can last three hours. A post-surgery hospital stay is required, and it generally takes several weeks to resume normal activities.
In some cases, the surgeon may choose to completely remove the disc and fuse the vertebrae around it, but this is usually a last resort. The fusion can cause undue stress on the spinal column and other discs because the fused vertebrae move in an irregular motion. Surgeries can range in cost from $20,000 for a microdiscectomy to upwards of $50,000 for the other surgeries mentioned.
Prevention Is The Best Medicine
It is important for patients to know the risk factors for developing a herniated disc:
- Age Discs lose water content as people age, so the disc becomes less flexible and more brittle and therefore more likely to rupture.
- Genetics definitely play a role and some people have a predisposition to developing these herniations.
- Weight is also a factor; if you’re overweight, you’re putting undue pressure on your discs.
- Work injury people who perform lifting as part of a job are at greater risk for back injury
Herniated discs are rarely caused by trauma. Instead, herniated discs occur over time; most people cannot recollect a single event that caused the herniated disk. Ruptured discs need time to properly heal, and the type of treatment to help the healing process should be determined by both you and your physician.
Prevention is always best, and to keep your back healthy, maintain a healthy weight and good posture, and exercise often to strengthen your torso and back muscles to better stabilize and support the spine. Lift properly, using your legs and not your back.
You may also like:
4 Nutrients That Help With Bone & Joint Health You May Not Know