The Biochemistry of Pain – What’s Going On Beneath the Surface?
Pain is a distressing feeling often caused by intense or damaging stimuli. The International Association for the Study of Pain’s widely used definition defines pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage”. In medical diagnosis, pain is regarded as a symptom of an underlying condition. Pain motivates the individual to withdraw from damaging situations and to protect a damaged body part while it heals.
We are all familiar with the distressing and uncomfortable feeling that pain brings. When pain occurs, we register it on a systemic or whole-body scale. We tend to think of pain as it affects a particular area of the body, such as back pain, neck pain or joint pain, but have you ever wondered what is going on inside your body when you experience pain? What’s the biochemical reaction that’s happening?
Below we’ll take a look at a few examples of pain, related to specific conditions and what’s actually going on physiologically within the body. Few of us tend to think of pain on a biochemical level, yet one of the keys to treating pain is understanding the internal inflammatory response that occurs.
There are many different pain syndromes: back pain, neck pain, arthritis, shoulder pain, migraine, neuropathic pain, fibromyalgia, shoulder pain, central pain, acute pain, chronic pain and more. Dull pain, sharp pain, tingling and aching all manifest differently, but at the same time have something in common. Even though there are different pain syndromes and different types of pain, the commonality among all of them is an inflammatory profile. This profile can vary from person to person and it can even be different in the same person at different times. In all cases, there is a unifying theory of pain: all pain originates with inflammation and the inflammatory response.
The underlying origin of pain is inflammation. Pain receptors are activated and pain signals are transmitted. On the biochemical level, there are several factors that are important: neurotransmitters, cytokines and growth factors, among others. All of these substances help cells signal each other and help tissues grow and heal. To show the underlying commonalities, let’s look at three of the most prevalent inflammatory pain syndromes.
Arthritis is characterized by joint inflammation and people of all ages can have it. There are many different forms of arthritis, but all forms are caused by inflammation which leads to the pain that is so characteristic of arthritis.
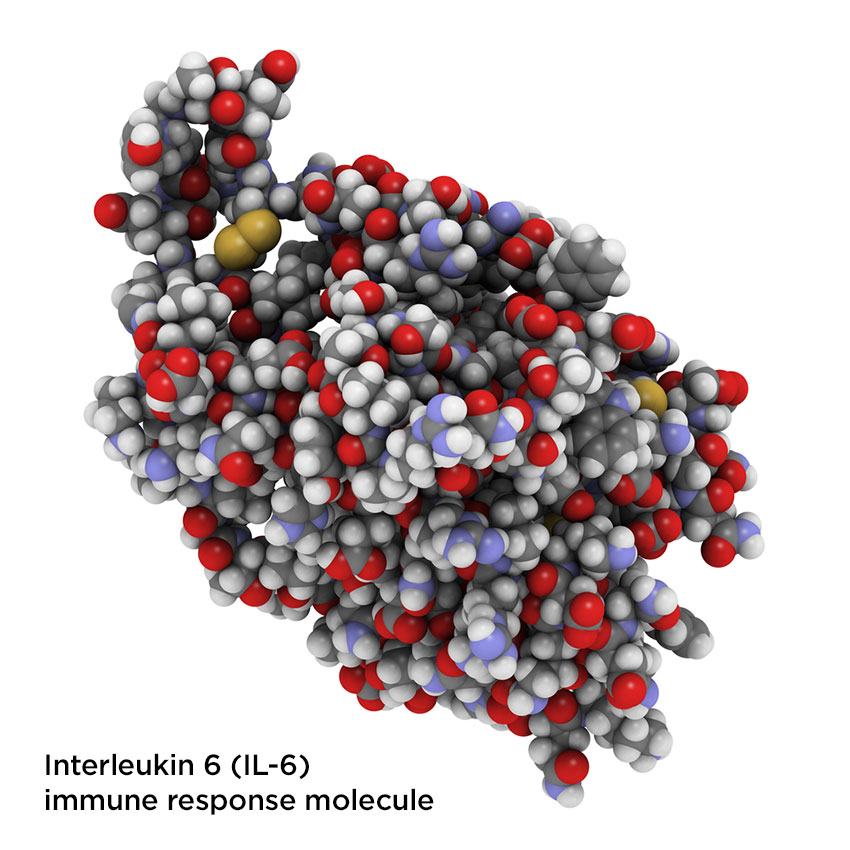
In people without arthritis, the cartilage is being constantly repaired by substances called cytokines. There is supposed to be a healthy balance between cartilage breakdown and cartilage synthesis. Yet in people with arthritis, a higher amount of cytokines that break down cartilage are routinely found around inflamed joints – substances like interleukin-1 (IL-1) and interleukin-6 (IL-6). Over time, as the cartilage erodes, progressive damage occurs, bones lose the shock-absorbing mechanism and painful bone-on-bone contact occurs.
Rheumatoid arthritis is an autoimmune disease in which the person’s immune system destroys its own joints. Patients with rheumatoid arthritis also have elevated interleukin-1 levels. Interleukins are proteins produced by the body’s immune cells (white blood cells called leukocytes) to help regulate immune responses. High interleukin concentrations point to inflammation that the body is having trouble regulating.
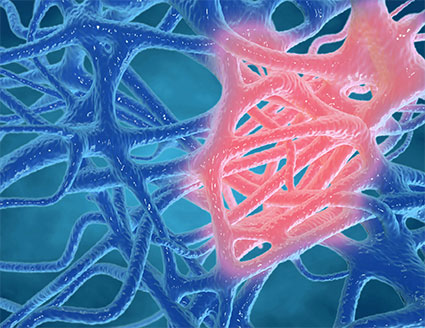
In patients with the chronic and painful musculoskeletal disorder known as fibromyalgia, widespread pain and morning stiffness is characteristic of the disease. While the origins of fibromyalgia are still not fully characterized, it is believed to be caused by neurogenic inflammation. The body has an inflammatory response to infection, allergens or other irritants, or even to emotional stress. Several studies have shown that patients with fibromyalgia have increased inflammatory transmitters, like interleukin-1R, -6 and -8. Interleukins are a family of proteins, and each one performs a different function. For example, IL-1R plays a major role in the central nervous system. Interestingly, IL-6 is known to create pain hypersensitivity and IL-8 is known to produce sympathetic pain, both hallmarks of fibromyalgia symptoms.
Neuropathic pain also acts very similarly in terms of inflammatory response. Nerve pain is characterized by increased sensitivity to a normal stimulus or by pain that results from a stimulus that usually does not cause pain. When nerve injury occurs, cells release a very high amount of IL-6, which may explain the hypersensitivity to pain. And when stress accompanies any pain syndrome, which it often does, the stress can further elevate levels of IL-1 and IL-6.
When the body is injured, cell membranes are damaged and injury disrupts the blood supply, so tissues may not get the oxygen they need. In response, the body reacts immediately by producing initial inflammation by releasing the same cytokines near the injury site. This causes an immediate tightening of the blood vessels to seal the injury. While this describes acute rather than chronic inflammation and only lasts a few days, the underlying inflammatory profile is the same as in the chronic conditions described above.
The inflammation works as it always does, triggering local nerve cells to send pain signals to the brain. When the inflammation is over, monocyte cells are sent in to clean up dead cells and other debris from the injury site.
Inflammation is the underlying factor in all of these pain scenarios. Furthermore, all treatments are based on determining the exact inflammatory profile and suppressing the production of cytokines and other inflammatory substances. This suppression is traditionally done pharmacologically with drugs like opioids that block the inflammatory substances, or by surgical intervention. These drugs act more generally; in reality, there are very few drugs that respond to specific biochemical mediators. These drugs simply do not exist, so doctors are left to prescribe drugs like opioids which have unwanted side effects and can lead to addiction.
You may also like:
Orthopedic Surgeons Seek Opioid-Alternatives For Pain Management
Interventional or Non-Interventional Pain Management: What’s The Difference?